Description of Cataract Surgery
The vast majority of cataract surgery performed in the United States today is completed using the phacoemulsification technique (also referred to as phaco). On rare occasions, traditional ECCE may still be used. In addition, retinal sub-specialists occasionally remove cataracts with a Fragmatome, which involves a slightly different type of ultrasound procedure, and it is reserved mainly for patients who are not good candidates for phacoemulsification. Because the vast majority of cataracts are removed using the phacoemulsification technique, the following description is for phacoemulsification surgery only.
The Phacoemulsification Procedure
Upon reaching the operating room, you will be placed on heart, blood pressure and oxygen monitors. Cataract surgery is performed in a sterile fashion, so your eye will be cleaned and sterilized. Following that, a sterile drape will be placed over your face with an opening only for your eye. Rest assured, you will have plenty of oxygen during the time you are under the drape.
Once you are draped, your surgeon will begin your procedure. If you are feeling anxious under the drape, let your doctor know; the anesthesiologist can give you medicine for this, which will help you to relax, rest, and remain still while your surgeon works. Many surgeons will explain the various steps of the procedure to patients as they are being performed. This is not a good time to ask questions or to engage in conversation, however, because when you talk, your eye moves, which makes the procedure more challenging for your surgeon. You may feel cool liquid or some pressure in your eye, but you should not feel pain. If you have discomfort, let your surgeon know, but otherwise, try to remain quiet. You may also see some bright and/or colorful lights during the procedure. This is normal and is not cause for concern.
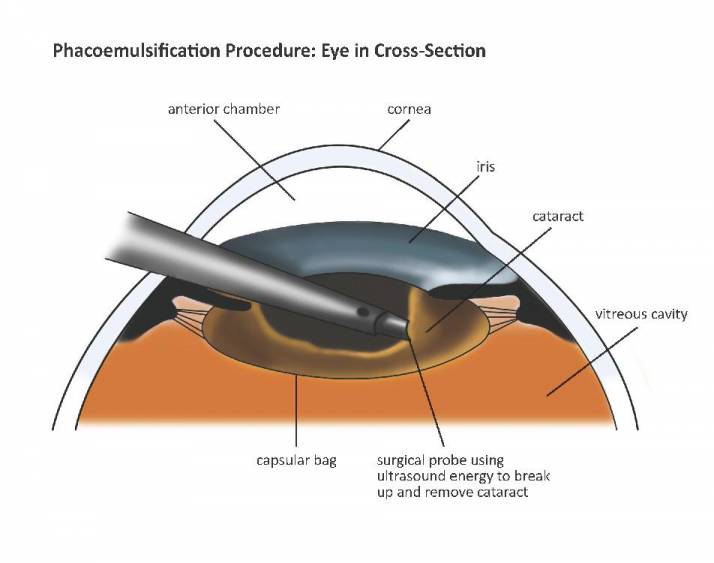
Your surgeon will place a lid speculum in your eye to keep it open during surgery. A small 2–3 mm incision in the peripheral cornea is then created. Following this step, your surgeon may inject some local anesthetic into the eye to help numb it. This may cause a bit of burning, but should resolve quickly. The anterior chamber will then be filled with a thick, jelly-like substance that helps your eye stay formed during the procedure, and protects the inner layer of the cornea. Your surgeon will then use special instruments to create a circular opening in the anterior capsule, called the capsulorrhexis. This allows your surgeon access to the cataract, which is housed in the capsular bag. Following this step, the central nuclear cataract will be fragmented with ultrasound, and then removed with an aspirating cannula. After nucleus removal, the cortex will be removed by aspiration through a small-tipped cannula.
Illustration showing phacoemulsification of a brunescent cataract.
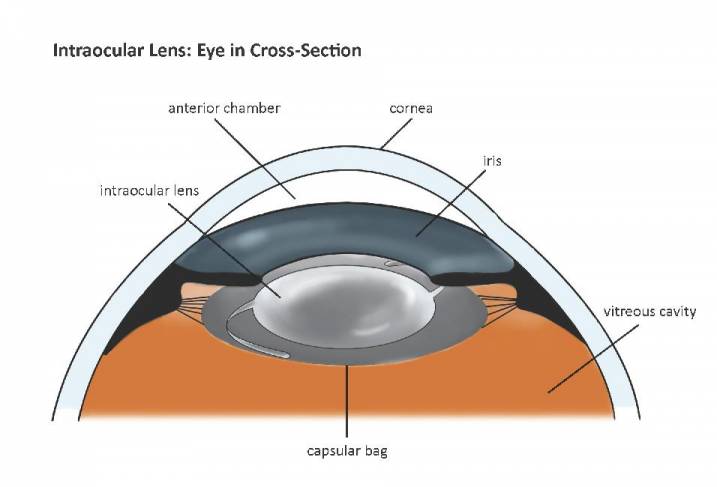
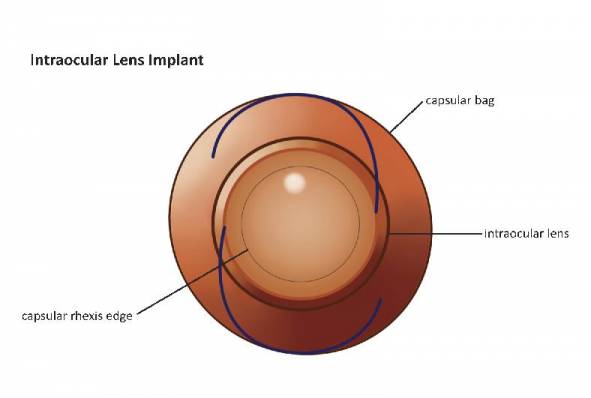
This completes the removal of your cataract. Now, your eye must be prepared for your IOL. The capsular bag deflates after the large cataract is removed, so your surgeon will inject more specialized jelly into the capsular bag to expand it. Following this step, your folded intraocular lens will be placed and positioned in the capsular bag. Occasionally, the lens is placed in front of the bag, or in front of the iris if the capsular bag cannot adequately support the IOL. Following placement in the eye, the IOL will unfold, and its position will be refined.
Following IOL insertion, the remaining jelly will be removed with an aspirating cannula. Your surgeon will then check your incision to make sure it is sealed. If there is slight leakage of fluid, your surgeon will place a stitch to seal it. Occasionally, there are other reasons to place a stitch; if you fall into one of these categories, your surgeon will let you know. However, the vast majority of corneal incisions for cataract surgery are self-sealing and do not require stitches. If you do need to have a stitch placed, it is usually removed at your one-week postoperative visit. Your procedure is now complete.
The surgical procedure itself takes only 10–20 minutes if there are no extenuating circumstances. However, if your eye is complicated, or you are having multiple procedures performed at the same time, the surgery will take longer. Every eye and every recovery are different, so try not to compare your surgery to that of someone else you know.
Illustration showing intraocular lens in the capsular bag after cataract removal.
Illustration showing direct view of intraocular lens in the capsular bag after cataract removal.
Instructions Following Cataract Surgery
After your procedure, your surgical drape will be removed, antibiotic and anti-inflammatory drops will be placed in your eye, and a clear hard shield will be placed over your eye. You will then be taken to the recovery room or the post-anesthesia care unit. There, you will be given something to drink. Once the anesthesiologist has determined you are stable to be discharged, you will be able to leave with your driver. You will usually receive an “eye kit”, including tape for your eye shield, some artificial tears, and your postoperative instructions. The nurse will go over these instructions with you and, if you wish, with whoever has come with you to the surgery center. It is very helpful to have a friend or family member hear these instructions, as you may be a bit forgetful immediately following anesthesia. Every surgeon will have his or her own individual set of instructions, so be sure to follow your particular surgeon’s instructions after surgery, as they will be adjusted for your specific eye surgery. If you have additional questions about your surgery or what to do following your surgery, be sure to ask these questions and write down the answers so you can refer back to them at a later time.
© Vision Information Services, LLC, Mooresville, NC 2012